Superior Labral Tear
of the Shoulder (SLAP)
Superior Labral Tear
of the Shoulder (SLAP)
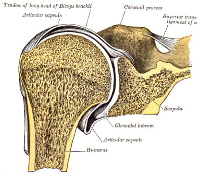
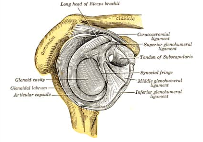
Anatomy
The shoulder joint involves three bones: the scapula (shoulder blade), the clavicle (collarbone), and the humerus (upper arm bone). The humeral head rests in a shallow socket on the scapula (glenoid). Because the head of the humerus is much larger than the glenoid, a soft fibrous cartilage ring called the labrum surrounds the rim of the glenoid to help deepen the socket; the labrum also helps to stabilize the shoulder joint. The labrum deepens the glenoid by up to 50 percent so that the head of the humerus fits better. In addition, it serves as an attachment site for several ligaments.
Injuries
Injuries to the labrum can occur from trauma or repetitive stressful shoulder motion. Examples of traumatic injury include:
- Falling on an outstretched arm
- Forcefully directed blows to the shoulder
- Sudden pull, such as when trying to lift a heavy immobile object
- Forceful overhead motions
Tears can be located either above (superior) or below (inferior) the middle of the glenoid. A SLAP lesion (superior labrum – anterior [front] to posterior [back]) is a tear of the labrum above the middle of the glenoid that may also involve the attachment point of the biceps tendon; the tear may extend into the biceps tendon substance. A tear of the labrum below the middle of the glenoid socket that also involves the inferior glenohumeral ligaments is called a Bankart lesion. Tears of the glenoid labrum often occur in conjunction with other shoulder injuries, such as a dislocated shoulder (full or partial [subluxation]).
Signs and symptoms
It is difficult to diagnose a tear in the glenoid labrum because the symptoms are very similar to other shoulder injuries or degenerative conditions. Symptoms include:
- Pain, usually with overhead activities
- Catching, locking, popping, or grindings
- Occasional night pain or pain with daily activities
- A sense of instability in the shoulder
- Decreased range of motion
- Loss of strength
Treatment
Until the final diagnosis is made, your doctor may prescribe anti-inflammatory medications and rest to relieve the symptoms. Rehabilitation exercises to strengthening the the muscles of the rotator cuff and the rest of the shoulder girdle (scapula,arm,neck,chest, and back) are often recommended. If these conservative measures are insufficient to alleviate the symptoms and restore normal function, your doctor may recommend arthroscopic surgery.
During the surgery, your doctor will perform an arthroscopic evaluation of the labrum, biceps tendon, and rotator cuff. If the injury is confined to the labrum itself and does not involve the biceps tendon (and the biceps tendon attachment is “stable”), your doctor will remove the torn tissue and correct any other associated problems. If the tear extends into the biceps tendon or if the biceps tendon is detached (unstable), your doctor will need to repair and reattach the biceps tendon. Sometimes the biceps tendon is too damaged to be repaired, and it must be re-positioned away from the shoulder joint to prevent future or continued pain and mechanical symptoms. If the labrum tear is below the middle of the glenoid, your doctor will reattach the labrum and associated ligaments back to the glenoid rim (Bankart repair).
Rehabilitation
After surgery, you will need to keep your shoulder in a sling for a minimum of 3-4 weeks. Your doctor will also prescribe gentle, passive range-of-motion exercises. When the sling is removed, you will need to do motion and flexibility exercises and eventually start strengthening. Athletes can usually begin doing sports-specific exercises after 12 weeks, although it is generally approximately 6 months before the shoulder is fully healed.